Glaucoma- The Silent Thief of Sight

Last Sunday evening, I had a frightening experience with my eyes. As I stepped inside the house, I saw a mass of small black dots floating across my left eye and a flash of white light in my far peripheral vision. This was followed by a sharp headache on the left side of my head. I panicked and left a brief message on my ophthalmologist’s office phone, letting her know that I needed the first appointment ASAP on Monday. I applied an ice pack to my head and eyes, and I kept my eyes closed for the rest of the evening into the night. As I was lying in bed that night, I kept thinking about my sister and dad, both had diabetes and glaucoma, and I wondered if I was the latest victim of the silent thief of sight.
The ophthalmologist’s office called early on Monday for me to come in for a visit. After a thorough dilated eye examination, she found no tears or damage to the eye or retina. I was sent to the retinologist for further evaluation that day because I complained about seeing the flash of white light. The retinologist report also came back clean. The experience was so frightening that I vowed that an eye care plan will become a part of my self-care routine.
What is Glaucoma
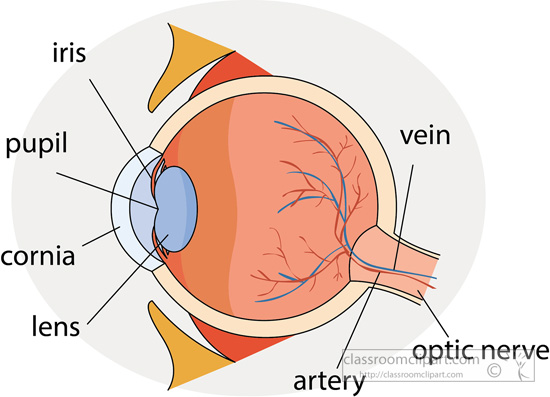
Glaucoma is known as the silent thief of sight. The term glaucoma refers to a group of eye disorders that leads to progressive damage to the optic nerve and result in vision loss and blindness. Having diabetes increases the odds of someone developing glaucoma, a condition in which there is a slow buildup of fluid pressure in the eye, which subsequently damages the optic nerve. According to the American Optometric Association, not everyone with high eye pressure will develop glaucoma. Some people with normal eye pressure can also develop glaucoma because when the pressure inside a person’s eye is too high for a particular optic nerve, whatever that pressure measurement may be, glaucoma will develop.
There are typically no warning signs or symptoms of glaucoma. Most people do not notice a change in their vision because the initial loss is the side or peripheral vision, and the visual acuity and sharpness of vision is maintained until late in the disease. Open-angle glaucoma is the most common form of the disease. In open-angle glaucoma, the angle in the eye where the iris meets the cornea is normal, but the eye’s drainage canals become clogged over time. The clogged canal causes the internal eye pressure to increase, which subsequently damages the optic nerve, leading to blindness.
Who is at risk?
The National Eye Institute states that glaucoma is the seconding leading cause of blindness in the US and the following groups of people are at risk:
• People over 40 specifically African Americans
• Hispanics over the age of 60
• Persons with a family history of glaucoma
• Having medical conditions such as diabetes, high blood pressure, and heart disease
• Physical injuries to the eye, such as severe trauma from a hit in the eye. Damage to the eye can result in the dislocated of the lens, closure of the drainage angle, and internal injury to the area, all of which can contribute to the increase in eye pressure
• Other risk factors include thinner corneas, chronic eye inflammation and taking medications that increase the pressure in the eyes
• Corticosteroid use for a prolonged period appears to put people at risk of getting secondary glaucoma. (Secondary glaucoma refers to any form of glaucoma in which there is an identifiable cause of increased eye pressure, resulting in optic nerve damage and vision loss).
While glaucoma cannot be prevented, if it is diagnosed and treated early, it can be controlled. To prevent or slow further vision loss, medication or surgery may be options for some persons. The critical point to note is that vision already lost to glaucoma cannot be restored.
Can glaucoma be prevented?
The Glaucoma Research Foundation stated that the best form of prevention against significant glaucoma damage is regular eye examination, which includes a comprehensive dilated eye examination. Early detection is, therefore, the key. Checks for glaucoma should be done before age 40, every two to four years
• from age 40 to age 54, every one to three years
• from age 55 to 64, every one to two years
• after age 65, every six to 12 months
Anyone with high-risk factors should be tested every year or two after age 35. Those at higher risk include people of African descent, people with diabetes, and people with a family history of glaucoma. You are at increased risk if you have a parent, brother, or sister with glaucoma.
Exercise
An exercise program that includes walking, jogging three or more times per week can help to lower intraocular pressure (IOP) and prevent damage to the optic nerve. The Glaucoma Foundation, however, cautions against inverted yoga positions such as headstand and shoulder stand as these positions increase IOP.
Protective Eyewear/Sunglasses
Protect your eyes when engaging in sports, outdoor activities, or home improvement projects as any trauma to the eye can increase eye pressure and cause internal eye damage. Other preventative measures include not smoking, maintaining a healthy weight, and eating a varied and healthy diet- a diet that is rich in dark leafy greens and brightly colored vegetables.
Since I’m 55 years old and I had a sister AND a parent with diabetes and glaucoma, my retinologist has added the extra step of scheduling me to see him in 3 months for a follow-up review. I’m more than happy to comply with his recommendation.
Photo credit: Photo by Ben Spin from FreeImages
Sources: https://www.allaboutvision.com/conditions/glaucoma.htm
National Eye Institute: https://www.nei.nih.gov/
Glaucoma Research Foundation: https://www.glaucoma.org/glaucoma/
America Glaucoma Society: https://www.americanglaucomasociety.net/home